Key Takeaways:
- Treponema pallidum is a spirochete bacterium that causes syphilis, bejel, and yaws in humans.
- It is usually found in lesions on the genitals, mouth, lips, fingers, and other areas during primary and secondary syphilis.
- Darkfield microscopy of fluid from lesions can directly detect the presence of the spiral-shaped Treponema pallidum bacteria.
- Serologic blood tests look for antibodies produced in response to T. pallidum infection rather than detecting the bacterium itself.
- Prenatal screening and newborn physical exams help detect congenital syphilis acquired from an infected mother.
- Are the Sides of a Right Angled Triangle Equal?
- What Is the Fascinating History of the Bearskin Hat?
- What Do Yeti Numbers Mean?
Introduction
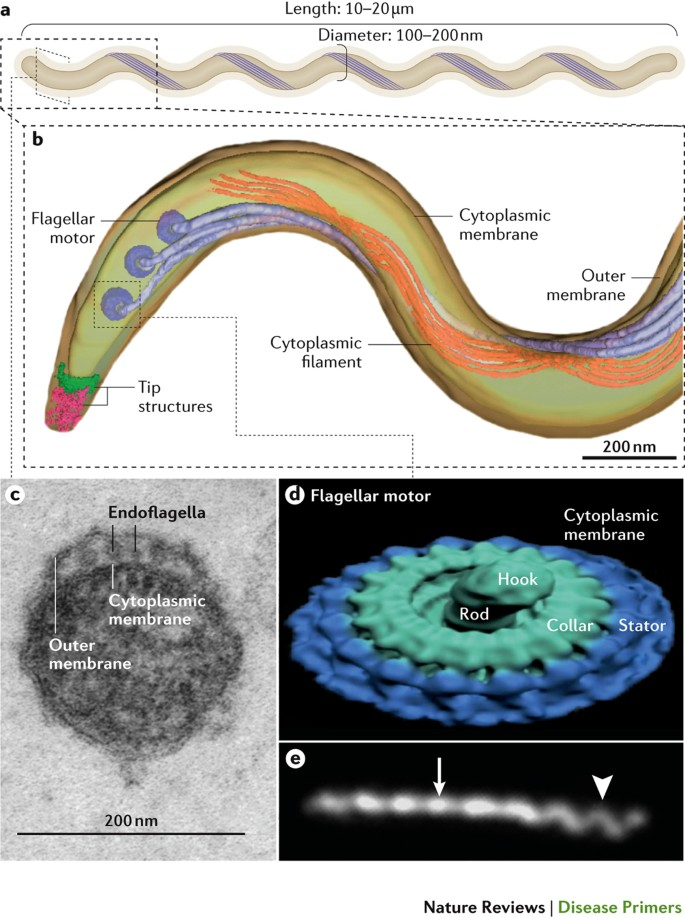
Syphilis and related diseases have afflicted humankind for centuries, but it was not until the early 1900s that scientists were able to identify the causative agent, Treponema pallidum. This corkscrew-shaped bacterium continues to impact global health today. Understanding where T. pallidum is found in the body can aid clinical diagnosis and help control the spread of syphilis and other treponemal diseases.
This comprehensive article will analyze the typical locations where Treponema pallidum occurs during the progression of syphilis infection. It covers how darkfield microscopy and serologic blood tests detect the presence of the bacterium in different body sites. The value of prenatal screening and newborn exams for identifying congenital syphilis will also be discussed. Readers will gain valuable insights into where T. pallidum manifests during the course of infection and how healthcare providers test for the bacterium.
Where Is Treponema pallidum Found at Different Stages of Syphilis??

The locations where Treponema pallidum resides in the body vary as syphilis progresses through its primary, secondary, latent, and late stages. Understanding this pattern of dissemination helps inform clinical diagnosis.
In Primary Syphilis Lesions
During the first stage of syphilis infection, T. pallidum rapidly multiplies at the site of initial inoculation, usually causing a firm, painless lesion called a chancre to appear. The bacteria remain concentrated in this primary syphilitic lesion.
Common locations for primary chancres include:
- The genitals, such as on the penis, labia, vagina, cervix, or anus
- The mouth or lips
- Fingers
- Breasts
- Other sites of sexual contact
Darkfield microscopy of fluid from a suspected primary chancre can directly visualize the spiral-shaped T. pallidum bacteria under the microscope. This definitive diagnostic method takes advantage of the bacteria’s concentration in the lesion exudate.
Widespread Dissemination in Secondary Syphilis
After 1-2 months, the primary chancre resolves even as T. pallidum spreads through the body. This triggers the generalized secondary stage of syphilis. The bacterium can now be found in many bodily locations:
- Skin rashes and mucocutaneous lesions on the trunk, limbs, palms, and soles
- Condyloma lata lesions in warm, moist areas like the perineum
- Patchy alopecia (hair loss) of scalp, eyebrows, beard area
- Conjunctivitis and uveitis of the eyes
- Generalized lymphadenopathy
- Hepatic, renal, or splenic involvement
- Osteitis and osteochondritis
- Meningitis and cerebrospinal fluid abnormalities
Scrapings from moist secondary lesions can be examined under darkfield microscopy for the presence of T. pallidum. In blood and spinal fluid, the bacteria are sparse and harder to visualize.
Latent and Late Stages: Harder to Detect
After the secondary stage, T. pallidum infection enters an asymptomatic latent period where the bacteria persist but are kept in check by immune responses. The location of the bacteria during latent syphilis is poorly characterized.
In tertiary or late syphilis, which develops in about one-third of untreated cases, the bacteria can again be found in characteristic granulomatous lesions of the skin, bones, and viscera. Darkfield examination of exudates from gummas and other moist lesions can reveal T. pallidum.
Congenital Syphilis in Newborns
Treponema pallidum can also be passed from an infected pregnant woman to her fetus via the placenta, resulting in congenital syphilis. T. pallidum is often found in the placenta, umbilical cord, and other fetal organs after birth.
Careful physical examination of newborns along with darkfield microscopy of suspicious lesions, nasal discharge, or autopsy specimens can help diagnose congenital syphilis.
How Do Tests Detect Treponema pallidum at Different Locations??
In addition to darkfield microscopy, other diagnostic approaches exploit the varying dissemination of T. pallidum during syphilis infection.
Darkfield Microscopy
As discussed earlier, darkfield microscopy of exudates from primary or secondary syphilitic lesions provides a definitive diagnosis by directly visualizing the spiral-shaped, actively motile T. pallidum bacteria. The corkscrew motion and thin, delicate morphology distinguish them from other spirochetes.
A 2017 study found that sensitivity of darkfield microscopy was 75% for primary syphilis and 81% for secondary syphilis when adequate lesion exudate was obtained. However, the technique requires specialized equipment and training.
Serologic Blood Tests
Instead of detecting T. pallidum itself, serological blood tests identify antibodies produced in response to syphilis infection. During primary syphilis, antibodies are initially directed against T. pallidum surface proteins.
As infection progresses, antibodies develop against cardiolipin and lecithin released from damaged host cells, detected via rapid plasma reagin (RPR) testing. RPR titers correlate with disease activity.
The most specific serologic tests look for IgM and IgG antibodies to T. pallidum antigens like TP-47, TP-15, and TP-17. Reactive treponemal tests indicate past or present syphilis infection.
Polymerase Chain Reaction (PCR)
The low concentration of T. pallidum in blood and spinal fluid during latent and late-stage syphilis makes PCR an appealing diagnostic approach. PCR amplifies and detects treponemal DNA in clinical specimens.
However, PCR results correlate poorly with disease stage and standard serologic testing. The clinical utility of PCR for diagnosing syphilis remains uncertain at this time.
Direct Fluorescent Antibody Test
Direct fluorescent antibody staining of smears from primary or secondary lesions uses fluorescein-tagged anti-T. pallidum antibodies to visualize the bacteria via fluorescent microscopy. It offers definitive diagnosis like darkfield testing but is rarely performed today.
Biopsy Immunostaining
Immunohistochemical staining can detect T. pallidum antigens in tissue biopsy specimens, including placenta and umbilical cord. However, biopsying is invasive and not routinely indicated.
Prenatal Screening
Screening pregnant women via nontreponemal and treponemal antibody tests facilitates early syphilis treatment to prevent congenital syphilis. All women should be screened upon first prenatal visit.
High-risk pregnant women should be repeatedly screened throughout pregnancy and at delivery. Positive results warrant evaluation of the newborn.
Newborn Physical Exam
Careful examination of newborns born to syphilis-seroreactive mothers can reveal signs of congenital syphilis like hepatosplenomegaly, jaundice, condylar hypertrophy, maculopapular rash, rhinitis, or pseudoparalysis.
Lesions and body fluids should be tested via darkfield microscopy, PCR, or direct fluorescent antibody staining to detect T. pallidum.
Conclusion: Widespread Dissemination During Secondary Syphilis
In summary, Treponema pallidum manifests at specific body sites during the course of syphilis infection. The bacterium concentrates at the initial inoculation lesion in primary syphilis. Darkfield microscopy of exudates offers definitive diagnosis.
In secondary syphilis, T. pallidum spreads hematogenously, and serologic antibodies become detectable. The bacteria can be found in myriad locations throughout the body during this stage.
Latent and late syphilis feature more limited dissemination. Congenital syphilis involves transmission to the fetus during pregnancy. Tests like darkfield microscopy, serology, PCR, and immunohistochemistry identify T. pallidum by exploiting its distribution in the body. Understanding where the bacterium resides aids clinical diagnosis and public health control of these debilitating diseases.
Frequently Asked Questions
What diseases are caused by Treponema pallidum?
Treponema pallidum subspecies pallidum causes syphilis in adults as well as congenital syphilis in infants born to infected mothers. The bacterium also causes endemic syphilis (bejel) and non-venereal syphilis (yaws), depending on the geographic region.
How do people usually get infected with T. pallidum?
T. pallidum is usually transmitted sexually via direct contact with an infectious lesion on the genitals, mouth, lips, fingers, etc. Congenital syphilis occurs when an infected pregnant woman passes the bacteria to her fetus in utero. Non-venereal spread can occur under poor hygiene conditions.
Why is darkfield microscopy useful for diagnosing early syphilis?
Darkfield microscopy allows direct visualization of the live, motile, spiral-shaped T. pallidum bacteria in fluid from primary or secondary lesions. This provides a definitive diagnosis at a stage when the bacteria are concentrated locally before spreading through the body.
How long can T. pallidum survive outside the human body?
T. pallidum is extremely fragile and cannot survive more than a few hours outside of moist tissue within the human body. Drying, heat, oxygen, and disinfectants can all rapidly kill the bacteria on environmental surfaces.
What happens to T. pallidum during the latent stage of syphilis?
The location of T. pallidum during latent syphilis is not well characterized. The bacteria likely persist in a dormant state at low levels that evade immune detection. They may reside in lymph nodes, bone marrow, spleen, liver, or other tissues during latent infection.
Why is prenatal screening important for syphilis?
Screening pregnant women through nontreponemal and treponemal antibody tests identifies syphilis early so that antibiotic treatment can be provided. This prevents transmission of T. pallidum to the developing fetus and avoids devastating cases of congenital syphilis
- Are Hannibal and Will Lovers?
- How To Start A Ford F250 Without Key?
- When Asar Time Start?
- Can You See Who Reported You on TikTok?
- What Juice Is Good for Acid Reflux? [10 Best Juices]
- Should I Use a Shower Pouf?
- How to Craft Engaging, Comprehensive Articles with 5th Grade Readability
- Does Raiders Stadium Have Grass? An In-Depth Look at the Playing Surface
- What Blood Pressure Is Too Low? Everything You Need To Know
- Why Is My Guppies Back Curved?
- How to Start a Yoni Steam Business?
- How to Install Side Steps on Ford F150?
- Does Crying Burn Calories? (Detailed Guide)
- Are Corbin Seats Comfortable? An In-Depth Look at the Quality and Comfort of These Popular Motorcycle Seats