No, the atria (plural of atrium) do not contract at exactly the same time. There is a slight delay between the contraction of the right and left atria that allows blood to flow efficiently through the heart.
How the Heart Works
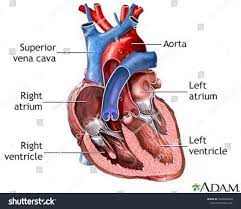
The heart has four chambers that work together to pump blood throughout the body. The two upper chambers are called the atria, and the two lower chambers are the ventricles.
The heart chambers contract in a coordinated sequence:
- First, the right atrium contracts and pushes blood into the right ventricle.
- Next, the left atrium contracts and fills the left ventricle with blood.
- Then the ventricles contract at nearly the same time to pump blood out of the heart.
This timed sequence allows the heart to pump blood efficiently with each beat.
- Are Git Submodules a Good Idea?
- Which Chakra do the Kidneys Come Under?
- What Does Foxglove Look Like? An In-Depth Examination
The Electrical Conduction System
The heart chambers contract in an organized manner because of the heart's electrical system. Special cells start the electrical signal that causes the muscle cells of the heart to contract.
The conduction system includes:
- The sinoatrial (SA) node – the heart's natural pacemaker located in the right atrium. It starts the electrical signal.
- The atrioventricular (AV) node – located between the atria and ventricles. It serves as the electrical bridge between the atria and ventricles.
- Bundle branches and Purkinje fibers – spread the signal quickly through the ventricles so they contract at nearly the same time.
This electrical conduction system coordinates the timed sequence of contraction that allows the heart to function efficiently as a two-stage pumping organ.
The Delay Between Atria and Ventricles
There is a slight delay between when the atria contract and when the ventricles contract. This delay is critical for effective heart function.
The atria contract first, ahead of the ventricles, for two key reasons:
- To fill the ventricles with blood. This ensures the ventricles have enough volume to pump out with each contraction.
- To prevent backflow of blood into the atria. The delay allows the atrioventricular valves to close before the ventricles contract.
The time delay between atrial and ventricular contraction is about 100 milliseconds or one-tenth of a second. This delay allows the atria to fill the ventricles passively just before the ventricles pump out blood.
- When Was the Omicron Variant of COVID-19 First Detected in the United States?
- Which Chakra do the Kidneys Come Under?
- Are Sequoias or Redwoods Bigger? A Comprehensive Comparison
Why Don't the Atria Contract at Exactly the Same Time?
While the ventricles contract almost simultaneously, there is a slight delay between contraction of the left and right atria.
This is because the electrical signal originates in the right atrium.
The SA node sends the electrical impulse first through muscle cells of the right atrium. This causes the right atrium to contract just before the left atrium.
The delay between the two atrial contractions is extremely short, lasting only 5-10 milliseconds. This allows the atria to fill the ventricles very quickly before ventricular contraction.
So in summary, the atria contract in rapid sequence, rather than simultaneously, because of the origin and conduction of the electrical signal through the heart.
What Would Happen if the Atria Contracted Simultaneously?
If the atria contracted at exactly the same time, it could disrupt coordination between the atria and ventricles.
Potential problems include:
- Incomplete filling of the ventricles. This could reduce the amount of blood pumped out to the body.
- Backflow of blood into the atria if they contract too early.
- Loss of the “priming” effect of passive ventricle filling just before they contract.
- Less efficient pumping.
Research in heart failure patients shows that loss of timing between atrial and ventricular contractions can significantly reduce the pumping efficiency of the heart.
So the short delay between right and left atrial contractions is an important part of the heart's coordinated timing that maximizes its function.
- How to Make Positrons?
- How to Become a Company Man in the Oilfield?
- What Does the Sternocleidomastoid Muscle Do?
Exploring the Electrical Conduction System In Depth
As described earlier, the electrical conduction system controls the timing of cardiac muscle contraction. Here is a more in-depth look at this system:
The SA Node
The SA node, located in the upper part of the right atrium, generates the electrical impulses that trigger heartbeats. It's considered the heart's natural pacemaker.
Features of the SA node:
- Initiates 60-100 impulses per minute in the average adult at rest
- Sends impulses to both atria through specialized conduction pathways
- Determines heart rate and adjusts it based on the body's needs
Loss of SA node function can occur in some heart conditions. This requires the heart's electrical system to rely on backup pacing sites.
The AV Node
The AV node is the only electrical connection between the atria and ventricles. It has two critical roles:
- Slow conduction – It slows down and regulates conduction of the impulse from the atria to the ventricles. This allows time for the atria to contract and fill the ventricles before they pump out blood.
- Block extraneous impulses – It prevents extra electrical impulses from reaching the ventricles too rapidly. This ensures coordination of timing.
The Bundle Branches and Purkinje Fibers
After passing through the AV node, the electrical impulse travels down the bundle branches – one for the left ventricle, one for the right.
It then rapidly spreads through the ventricles via the Purkinje fibers, a specialized conduction network. This quick conduction results in nearly simultaneous contraction of ventricular muscle cells.
In summary, the heart's ingenious electrical system enables the sequential yet coordinated pumping action that allows optimal heart function beat after beat.
Disorders That Disrupt Electrical Conduction
Problems with the heart's electrical system can disrupt the timed contraction sequence between the atria and ventricles. Some examples:
Atrial Fibrillation
Atrial fibrillation is an irregular heart rhythm caused by chaotic electrical signals in the atria. It can result in:
- Irregular ventricular rhythm since impulses reach the AV node unpredictably
- Reduced atrial contraction that impairs ventricular filling
- Blood clot formation in the fibrillating atria
Heart Block
Heart block refers to blocking or delay of electrical signals traveling through the AV node. This can cause:
- Prolonged delay from atrial to ventricular contraction
- Slowed heart rate
- Missed heartbeats
Ventricular Arrhythmias
Arrhythmias originating in the ventricles, such as ventricular tachycardia, disrupt the heart's normal electrical sequence. This can lead to:
- Unsynchronized ventricular contractions
- Rapid heart rates
- Cardiac arrest
Treatment of these conduction abnormalities aims to restore synchronized electrical activation and contraction patterns in the heart.
- What Blood Pressure Is Too Low? Everything You Need To Know
- Who Invented the Airfoil? A Historical Summary of Key Contributions
- What is the Lysogenic Phage? An In-Depth Explanation
The Heart's Electrical Activity as Seen On an ECG
An electrocardiogram (ECG) records the heart's electrical activity using electrodes placed on the skin. Analysis of ECG tracings provides information about conduction sequences in the heart.
Key electrical events seen on an ECG:
- P wave – atrial depolarization (contraction)
- PR interval – conduction from atria through AV node
- QRS complex – ventricular depolarization (contraction)
- QT interval – ventricular repolarization (relaxation)
The organized pattern of P waves, followed by QRS complexes at regular intervals, represents coordinated electrical conduction through the heart.
Abnormal ECG findings like irregular rhythms, prolonged intervals, or missing/extra waves can indicate problems with the heart's electrical system. ECG is thus a useful diagnostic and monitoring tool.
Echocardiography to Assess Cardiac Timing
Echocardiography uses ultrasound to create images of the heart's anatomy and motion. It can help assess the synchronicity of atrial and ventricular contraction.
Echocardiography can reveal:
- Delayed emptying of the atria due to impaired relaxation
- Inadequate ventricular filling after atrial contraction
- Dyssynchronous ventricular contraction in some forms of heart failure
- Regurgitation through faulty heart valves that close too late
Cardiac MRI can also assess the coordination of contraction between chambers. Evaluating cardiac timing is important for diagnosing certain heart rhythm and structural disorders.
- Is Phosphate a Polyatomic Ion?
- What Is the Survival Rate for Turner Syndrome?
- Are Derivations Important for NEET?
Preserving Cardiac Conduction in Heart Surgery
Various heart surgeries carry a risk of disrupting the heart's electrical conduction system. This can impair coordinated contraction patterns post-surgery.
Some measures surgeons take to avoid conduction abnormalities after heart surgery include:
- Carefully examining the anatomy to identify conduction pathways.
- Avoiding incisions through key electrical structures.
- Checking conduction timing continuously during procedures.
- Implanting a permanent pacemaker if significant conduction loss occurs.
- Following ECG tracings closely after surgery.
Advances in surgical techniques now allow many heart operations to be performed without long-term disturbance of the heart's electrical system.
Conclusion
In summary, the heart's ingenious electrical conduction system enables sequential contraction of the four chambers, with a vital delay between atrial and ventricular contraction.
The atria contract just ahead of the ventricles, allowing them to completely fill the ventricles with blood right before the ventricular pumping action.
Within this sequence, the atria contract rapidly one after the other, rather than at exactly the same time. This coordination results from the origin and spread of electrical impulses through the heart.
This precisely timed activation sequence maximizes the heart's ability to pump blood efficiently to the vital organs and tissues of the body with each contraction.
- Does Algae Get Rid of Waste?
- When Do Pallbearers Carry the Casket?
- How to Replace the Door Handle on a Ford F250
- How Much Weight Can a Tacoma Tailgate Hold: A Comprehensive Guide
- What Does Hydration Percentage Mean?
- Can you see unsent messages on Instagram?
- Why Does Skin Lose Elasticity with Age?
- Can Maxillary Retention Cysts Cause Headaches?
- What Is Superselective Tace?
- How Long Do Seasonal Jobs Last at Amazon?
- Can You Jailbreak a Smart TV?
- Did Quintessential Quintuplets End?
- Are Bison Still Alive?
- Why Is My Cox Router Blinking Green?
- What's an Effect of Computerization on Workers?